Topic moisture associated skin dermatitis: Discover the essentials of Moisture Associated Skin Dermatitis, a prevalent condition, and explore effective strategies for prevention and management to ensure skin health and comfort.
Table of Content
- Types of MASD
- Prevention and Management Strategies
- Conclusion
- Overview of Moisture-Associated Skin Dermatitis
- What are the causes of moisture-associated skin dermatitis?
- YOUTUBE: Managing Moisture Associated Skin Damage
- Causes and Risk Factors
- Types of Moisture-Associated Skin Dermatitis
- Signs and Symptoms
- Diagnosis and Assessment
- Prevention Strategies
- Treatment and Management Approaches
- Home Care and Lifestyle Changes
- When to Seek Medical Attention
- Future Research and Developments
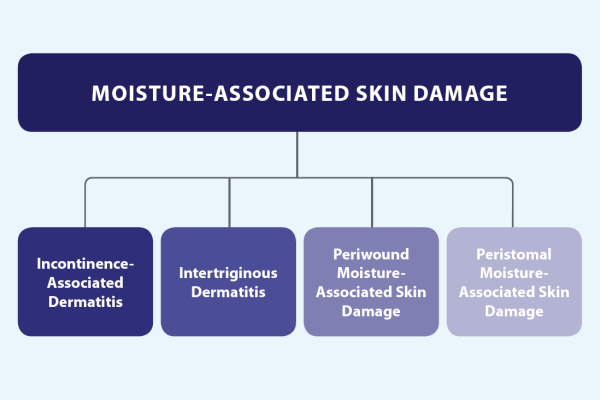
Types of MASD
- Incontinence-associated dermatitis (IAD): Caused by prolonged skin exposure to urine and stool.
- Periwound dermatitis: Associated with moisture from wound exudates.
- Peristomal dermatitis: Occurs around stoma sites due to exposure to bodily secretions.
- Intertriginous dermatitis: Develops in skin folds due to moisture, friction, and lack of air circulation.
READ MORE:
Prevention and Management Strategies
Preventive Measures
- Regularly changing incontinence products to keep the skin dry and clean.
- Applying barrier creams to protect the skin from irritants.
- Using gentle, pH-balanced cleansers for skin cleaning and avoiding harsh soaps.
- Ensuring proper skin drying with soft towels before applying any protective barriers.
Treatment Approaches
- Application of topical medicaments to reduce inflammation and promote healing.
- Implementing wound care practices for areas affected by periwound dermatitis.
- Adjustment of stoma appliances or use of specialized products to manage peristomal dermatitis.
- Employing absorbent fabrics and maintaining skin folds dry to address intertriginous dermatitis.
Conclusion
Effective management of Moisture-Associated Skin Dermatitis involves a combination of diligent preventive care and targeted treatment strategies to mitigate the effects of moisture on the skin. By understanding the different types of MASD and implementing appropriate care protocols, individuals can significantly reduce the risk of developing this condition and promote skin health.

Overview of Moisture-Associated Skin Dermatitis
Moisture-Associated Skin Dermatitis (MASD) is a significant skin condition characterized by inflammation and erosion caused by prolonged exposure to moisture. This condition affects various skin areas and can result from different moisture sources such as urine, feces, sweat, wound exudate, and saliva. MASD includes several subtypes, each related to the moisture"s origin, including incontinence-associated dermatitis, periwound dermatitis, peristomal dermatitis, and intertriginous dermatitis.
- Incontinence-associated dermatitis (IAD): This subtype is primarily caused by prolonged contact with urine and feces, leading to skin irritation and damage.
- Periwound dermatitis: Moisture from wound exudates can cause skin irritation and breakdown around wound sites.
- Peristomal dermatitis: Occurs around stoma sites, where moisture from bodily secretions can irritate and damage the skin.
- Intertriginous dermatitis: Develops in body folds due to a combination of moisture, friction, and reduced air circulation.
MASD"s impact on patient well-being and quality of life can be profound, emphasizing the need for effective prevention, timely diagnosis, and management strategies. Understanding the causes, risk factors, and varied manifestations of MASD is crucial for healthcare providers to develop comprehensive care plans that address both the symptoms and underlying causes of this condition.
What are the causes of moisture-associated skin dermatitis?
Moisture-associated skin dermatitis is caused by prolonged exposure to various sources of moisture. Some common causes of moisture-associated skin dermatitis include:
- Urinary or fecal incontinence, leading to exposure of the skin to urine or stool
- Perspiration, especially in areas where skin rubs together (intertriginous areas)
- Excessive wound exudate, which can irritate the surrounding skin
- Moisture around ostomy sites (peristomal moisture-associated dermatitis)
Managing Moisture Associated Skin Damage
Dive into the world of skincare and discover the secrets of maintaining optimal moisture levels for healthy, glowing skin. Learn effective tips and tricks to combat dryness and achieve a dewy complexion in just minutes!
Telling the difference: Differentiating between pressure injuries, IAD and Candidiasis
Unlock the power of differentiation in this captivating video that explores the importance of standing out in a crowded market. Gain valuable insights on how to set yourself apart and build a unique brand identity.
Causes and Risk Factors
Moisture-Associated Skin Dermatitis (MASD) is primarily caused by prolonged exposure to moisture, significantly affecting skin integrity. This condition can stem from a variety of sources, including urine, feces, perspiration, wound exudate, and saliva. Key risk factors contributing to the development of MASD include the chemical and physical properties of the moisture source, the skin"s prolonged contact with moisture, and individual health conditions that compromise skin integrity.
- Exposure to Bodily Fluids: Urine, feces, sweat, and other bodily fluids can irritate the skin and disrupt its natural barrier.
- Immobility: Limited mobility increases the risk of prolonged exposure to moisture, especially for individuals who are bedridden or use incontinence aids.
- Friction and Shear: Movement can cause friction and shear forces, exacerbating skin damage in moist areas.
- Poor Hygiene: Inadequate cleaning and drying of the skin can increase the risk of MASD.
- Medical Conditions: Conditions that increase the risk of incontinence or excessive sweating can contribute to the development of MASD.
Understanding these causes and risk factors is crucial for preventing MASD. It involves implementing strategies to reduce moisture exposure, protect the skin, and address underlying health issues that may increase susceptibility to the condition.

Types of Moisture-Associated Skin Dermatitis
Moisture-Associated Skin Dermatitis (MASD) encompasses several specific types, each resulting from different sources of moisture exposure. Understanding these types helps in diagnosing and tailoring treatment plans for affected individuals.
- Incontinence-Associated Dermatitis (IAD): This form is caused by prolonged skin exposure to urine and feces, leading to irritation and skin breakdown.
- Intertriginous Dermatitis: Occurs in skin folds where moisture, friction, and lack of air circulation contribute to skin damage.
- Periwound Moisture-Associated Dermatitis: Develops around chronic wounds where exudate causes skin irritation and breakdown.
- Peristomal Dermatitis: Affects the skin around stoma sites, caused by exposure to bodily secretions.
Each type of MASD requires a unique approach to management and prevention, focusing on controlling moisture exposure and protecting the skin barrier to promote healing and prevent further damage.
Signs and Symptoms
Moisture-Associated Skin Dermatitis (MASD) presents with distinct signs and symptoms that vary depending on the subtype and severity of the condition. Early recognition is vital for effective management and prevention of further skin damage.
- Erythema (Redness): A common sign, indicating irritation and inflammation of the skin.
- Itching: Often accompanies MASD, leading to discomfort and the potential for further skin damage due to scratching.
- Macération: Softening and breaking down of the skin due to prolonged moisture exposure.
- Pain or Burning Sensation: Can occur, especially in areas where the skin is particularly sensitive or damaged.
- Rash: May develop in affected areas, varying in appearance based on the individual"s skin type and the condition"s severity.
- Skin Erosion: The loss of the outer skin layer, leading to raw areas that may weep or bleed.
Identifying these signs and symptoms early can lead to prompt and effective treatment, reducing the risk of infection and further complications associated with MASD.
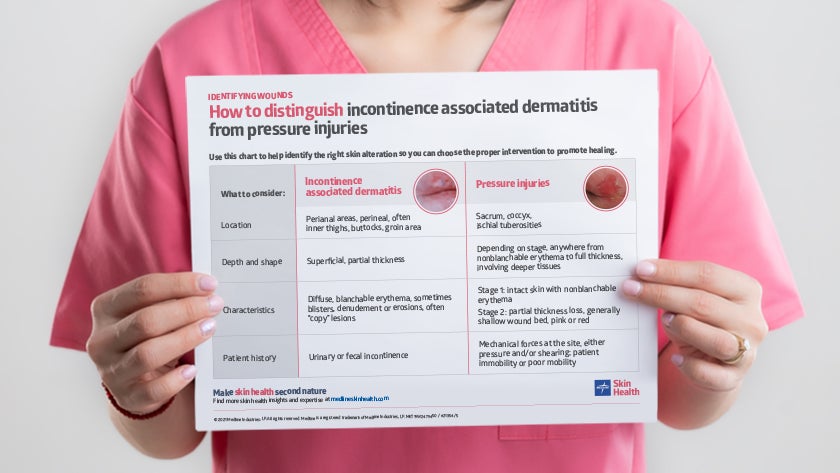
Diagnosis and Assessment
The diagnosis and assessment of Moisture-Associated Skin Dermatitis (MASD) require a careful and systematic approach. Healthcare professionals utilize a combination of clinical examination, patient history, and, in some cases, diagnostic tests to identify the presence and type of MASD. A thorough assessment helps in distinguishing MASD from other dermatological conditions with similar manifestations.
- Clinical Examination: Involves inspecting the affected skin areas for signs of erythema, maceration, erosion, and other characteristic features of MASD.
- Patient History: Gathering information about the patient"s medical history, including any underlying conditions, incontinence issues, and exposure to moisture sources, is crucial.
- Assessment Tools: Various scales and tools can be used to assess the severity of skin damage and the impact on the patient"s quality of life.
- Differential Diagnosis: It"s important to differentiate MASD from other skin conditions, such as fungal infections, by considering the pattern of skin damage and potential contributing factors.
Effective diagnosis and assessment are pivotal for developing an appropriate care plan, which includes interventions to manage moisture, protect the skin, and treat any underlying causes or complications associated with MASD.
Prevention Strategies
Preventing Moisture-Associated Skin Dermatitis (MASD) focuses on minimizing skin exposure to moisture and enhancing skin integrity. These strategies are vital for at-risk populations, including individuals with incontinence, limited mobility, or those recovering from surgery. Effective prevention involves a multifaceted approach tailored to individual needs and circumstances.
- Maintain Skin Cleanliness and Dryness: Regular cleansing with gentle, non-irritating products followed by thorough drying to remove moisture from the skin surface.
- Use Barrier Products: Application of barrier creams or ointments to protect the skin from irritants and moisture. Selection of appropriate products is key to effective skin protection.
- Manage Incontinence: Effective incontinence management using high-quality absorbent products and frequent changes to prevent prolonged skin exposure to urine and feces.
- Optimize Nutrition and Hydration: Adequate nutrition and hydration support skin health and resilience against moisture-related damage.
- Education and Awareness: Educating patients, caregivers, and healthcare providers about MASD risk factors, prevention strategies, and the importance of early intervention to prevent skin damage.
Implementing these strategies can significantly reduce the risk of developing MASD, improving patient comfort, and quality of life. Continuous assessment and adaptation of care plans are essential to meet the evolving needs of individuals at risk for MASD.

Treatment and Management Approaches
Treating Moisture-Associated Skin Dermatitis (MASD) involves a combination of medical interventions, skin care practices, and sometimes changes in lifestyle or environment. Effective management focuses on alleviating symptoms, healing the skin, and preventing future occurrences. Tailored approaches are necessary, considering the specific type of MASD and individual patient needs.
- Topical Treatments: Use of barrier creams, emollients, or medicated ointments to protect the skin and promote healing.
- Cleansing and Care: Gentle cleaning of affected areas with mild, non-irritating cleansers, followed by thorough drying to maintain skin integrity.
- Control of Moisture: Strategies to reduce skin exposure to moisture, including the use of absorbent products and frequent changes of incontinence aids.
- Environmental Adjustments: Modifications to living or care environments to reduce factors that contribute to moisture accumulation and skin damage.
- Diet and Hydration: Ensuring adequate nutrition and hydration to support skin health and resilience.
- Education and Support: Providing patients and caregivers with information on MASD prevention, symptom recognition, and care techniques.
Collaboration between healthcare providers, patients, and caregivers is crucial to develop and implement an effective management plan for MASD. Regular monitoring and adjustments to care strategies may be needed based on the patient"s response to treatment and changes in their condition or lifestyle.
Home Care and Lifestyle Changes
Managing Moisture-Associated Skin Dermatitis (MASD) effectively often includes adopting certain home care practices and lifestyle adjustments. These measures are aimed at reducing the risk factors for MASD, promoting skin health, and enhancing overall well-being.
- Regular Skin Assessment: Regularly inspect skin for any signs of moisture damage or irritation, especially in areas prone to wetness.
- Gentle Skin Cleansing: Use mild, pH-neutral cleansers and avoid rubbing the skin harshly. Pat the skin dry gently after washing.
- Moisture Barriers: Apply barrier creams or ointments to protect the skin from excessive moisture and irritants.
- Appropriate Clothing: Wear breathable, moisture-wicking fabrics to help keep the skin dry and reduce irritation.
- Hydration and Nutrition: Maintain a healthy diet and stay hydrated to support skin health and repair.
- Manage Incontinence: For individuals with incontinence, use high-quality absorbent products and change them frequently to minimize skin exposure to moisture.
- Environmental Control: Keep living areas well-ventilated and at a comfortable temperature to reduce excessive sweating.
These home care and lifestyle changes can be crucial in preventing MASD and maintaining skin integrity. Engaging in regular physical activity, when possible, and managing chronic health conditions effectively can also play a significant role in MASD prevention and management.

When to Seek Medical Attention
While many cases of Moisture-Associated Skin Dermatitis (MASD) can be effectively managed with home care and lifestyle adjustments, certain situations warrant professional medical evaluation and treatment. Recognizing when to seek medical attention is crucial for preventing complications and ensuring the best outcomes.
- Persistent or Worsening Symptoms: If symptoms do not improve with initial home care measures or if they worsen, it"s important to consult a healthcare provider.
- Signs of Infection: Redness, warmth, swelling, pus, or foul-smelling discharge from the affected area may indicate an infection requiring medical intervention.
- Severe Pain or Discomfort: Unmanageable pain or significant discomfort that interferes with daily activities is a sign that professional care is needed.
- Systemic Symptoms: Fever, chills, or other signs of systemic infection should prompt immediate medical attention.
- Impact on Quality of Life: When MASD significantly affects your quality of life or mental health, seek professional advice for more advanced treatment options.
Early intervention by healthcare professionals can prevent MASD from progressing and reduce the risk of secondary complications, such as infections or chronic wounds. A multidisciplinary approach involving dermatologists, wound care specialists, and primary care providers may be beneficial for comprehensive management of MASD.
READ MORE:
Future Research and Developments
Future research and developments in the field of Moisture-Associated Skin Dermatitis (MASD) are geared towards enhancing understanding, prevention, treatment, and management of this complex condition. With ongoing studies, the medical community aims to address knowledge gaps and improve patient outcomes.
- Understanding Pathophysiology: Greater focus on understanding the underlying mechanisms of MASD to develop targeted therapies.
- Advanced Materials for Skin Protection: Development of new barrier creams, dressings, and materials that offer better protection against moisture.
- Personalized Treatment Plans: Research into individualized care strategies based on patient-specific factors such as skin type, severity of symptoms, and underlying health conditions.
- Innovative Diagnostic Tools: Creation of advanced diagnostic tools for early detection and assessment of MASD, improving the timeliness and effectiveness of interventions.
- Educational Programs: Development of comprehensive educational programs for healthcare providers and caregivers to improve the prevention and management of MASD.
- Technology Integration: Incorporation of technology, such as telemedicine and mobile health apps, to support MASD management and patient education.
These future directions highlight the commitment to advancing care and support for individuals affected by MASD, with the goal of improving quality of life and reducing the burden of this condition.
With advancing research and comprehensive care strategies, the future for managing Moisture-Associated Skin Dermatitis looks promising, offering hope for improved outcomes and enhanced quality of life for those affected.

:max_bytes(150000):strip_icc()/peo-best-concealers-mature-skin-tout-562b727a81a14bc8a87df4d163d0b3cc.jpg)









:max_bytes(150000):strip_icc()/best-oils-for-skin-5088968-v1-a542b6a0c89d44bdbfb3258223afe30b.jpg)




